Two new training pathways have been developed for Allergy and Immunology:
- Allergy and Clinical Immunology (ACI)
- Allergy, Clinical and Laboratory Immunology (ACLI)
These pathways were implemented in August 2021, following GMC approval of the new curricula. The specialties will continue to be referred to as Allergy (ACI) and Immunology (ACLI) until the specialty name changes have been approved by the Department of Health.
The specialty of Allergy and Clinical Immunology (ACI) is the branch of medicine concerned with the body’s immune system. The clinical practice of this specialty encompasses clinical and laboratory activities dealing with the study, diagnosis, and management of patients with diseases resulting from disordered immunological mechanisms, (both deficient and exaggerated) and conditions in which immunological manipulations form an important part of treatment.
In the last three decades, there has been a significant increase in the requirement for allergy, clinical and laboratory immunology services. This is due to improved case ascertainment and treatment options for patients who have primary and secondary immune deficiencies (especially those caused by increased use of chemotherapy, immunosuppressive drugs, and biological agents). There has been a significant increase in the prevalence of allergic conditions and demand for allergy services with new and developing therapeutic intervention options in the fields of both allergy and immunology. There has been a corresponding requirement for immunology laboratories to provide support for primary care and secondary care in diagnosis and management of both allergic and immunological conditions.
Physicians in ACI specialise in the care of patients with heightened immune reactivity (allergy) and failure of the immune system (immunodeficiency).
As patient-facing clinicians, physicians in ACI are principally responsible for:
- Providing specialist allergy care services encompassing the assessment and management of patients with a broad spectrum of common atopic and allergic conditions (such as food, drug and insect venom allergy, anaphylaxis, asthma, eczema, rhino-conjunctivitis, and urticaria and angioedema),
- Providing clinical immunology services encompassing the assessment and management of patients with immunological conditions such as primary immunodeficiency and disorders of immune dysregulation
- Working closely with primary care, paediatricians, and other hospital specialists to manage patients with allergic and immune-mediated disease.
*The above information is credited to the JRCPTB. A link to their website can be found below.
Further information
General / application queries
For general queries relating to areas such as eligibility criteria, making an application or the Oriel system, please contact the Physician Specialty Recruitment Office.
Queries regarding the progress of a submitted application should be directed to the lead recruiter for this specialty:
| London and KSS (LaKSS) Recruitment | ||||||
|---|---|---|---|---|---|---|
| HST/general queries | General enquiries - Enquiry Form | |||||
| Fitness to practise - confidential | Fitness to practise form | |||||
Group 2 specialty
This is a Group 2 specialty and requires completion of the first two years of the internal medicine training (IMT) stage 1 programme or equivalent. Please visit the am I eligible? section of this website for further information about the eligibility criteria for Group 2 specialties.
Please be aware that this specialty accepts applicants from paediatrics training routes, in addition to core-level physician training.
Non-physician applicants must have obtained the basic specialty professional examination in addition to specific clinical experience and competences to be eligible.
Please view the specialty's person specification for information about the requirements for applying from a non-physician background and the deadlines for when this must be achieved.
Commitment to specialty
The specialty will be assessing your commitment to specialty as part of the shortlisting process. Please visit the application scoring page for more information about how this is assessed and scored.
This specialty does not require you to load documentary evidence to demonstrate your commitment; this will be assessed via your application form.
Joint allergy-immunology interview
The specialties of allergy and immunology - both of which will have recruitment managed centrally by London and Kent, Surrey & Sussex - hold a joint interview process.
Regardless of whether a candidate applies to the specialty of allergy or to immunology (or to both), they will sit one single joint interview; the assessment from which can be used to ascertain their suitability and readiness for progression to a post in allergy and/or immunology.
Interview Content
The interview will be split across two separate stations with a separate pair of interviewers scoring you on the areas within their station. There will be four questions, 10 minutes each in length. You will be marked on these questions, giving four scored areas in total. The headings below show the question areas and in which station they will be covered, along with information about what will be assessed.
Each station will last 20 minutes, so including the time between stations, the interview will be approximately 45-50 minutes.
Please note that this is subject to change and will be confirmed by the date of interview.
Prior to this question you will be given a clinical scenario and a short while to review it. You will then be asked questions relating to this scenario. This question will last approximately 10 minutes.
The clinical scenario will be relatively brief (two/three sentences), so once you have seen this, the remainder of the preparation time will allow you to undertake some short mental preparation. Whilst it is permitted to make notes, these must be destroyed as soon as your interview is completed and not shared with anyone.
Clinical scenario considerations
The scenario will describe a hypothetical clinical situation which has arisen in which you are, or have become, involved. Some points to consider when reviewing the scenario and preparing for discussion are:
- what steps you would take
- any potential treatments possible
- any further information you would gather
- how you would go about communicating with any people (eg patients, family members, colleagues) involved in the scenario
You should also consider any other factors you deem appropriate, using your experience and professional judgement.
This question will be a discussion of professionalism and governance.
This discussion will be prompted by a short question (often a single sentence) provided by interviewers. This will not be given to you before - this will be given verbally by interviewers once the previous question is finished. This question will last approximately 10 minutes
This section of the interview is designed to assess your demonstration and understanding of professionalism and governance in a given situation.
Familiarise yourself with Good Medical Practice
Please note - assessment here is underpinned by the principles of GMC Good Medical Practice.
You will need to give a presentation on the following topic, for no more than five minutes:
'An interesting research paper covering a recent development/research finding relevant to allergy and/or clinical immunology'
When preparing your presentation, please bear in mind the points below:
- Clarity & relevance most important - Select a topic that is relevant to the specialty, and which you can present with clarity. This is more important than trying to impress by choosing a subject that is esoteric or complex. It should be relevant to your application where possible.
- Five-minute time limit - Your presentation must last for no more than five minutes. Bear in mind that interviewers will be assessing the level, depth and content of your presentation, as well as expecting some structure.
-
No aids/resources allowed – you are not allowed to use any visual representations, such as PowerPoint, when giving your presentation and you must not share your screen. You are welcome to use prompts on small cards, but these should be for your own use only.
Post-presentation discussion
Once your presentation is finished (interviewers will stop you at the five minute-mark), interviewers will discuss it with you and ask further questions relating to the items you raise and any further points.
This discussion will take place for approximately five minutes.
This question will focus on your suitability for and commitment to training in the specialty and give you opportunity to expand on the information provided in your application form.
This question will last approximately 10 minutes.
Scoring framework
The score of 1-5 an interviewer will award you for each assessment area is judged in relation to how well you perform against an expected level. Below is the framework used to award scores at interview, as well as interpretation of what these scores represent:
|
Mark
|
Rating
|
Assessment
|
|
1 |
poor |
not considered appointable |
|
2 |
area for concern |
performed below the level expected from a core level trainee applying to the specialty; |
|
3 |
satisfactory |
performed at the level expected of a core level trainee applying to the specialty; |
|
4 |
good |
above average ability; |
|
5 |
excellent |
highly performing trainee; |
As shown in the table, for each of the question areas at interview, 3/5 is considered a satisfactory score; and reflects the level of performance that would be expected of a trainee ready to progress to a specialty training programme.
Should your performance go above and beyond this expected level, interviewers can award marks of 4/5 or 5/5 as appropriate.
Conversely, should your interview performance not reach the expected level, then interviewers can award marks of 1/5 or 2/5, as reflects their level of concern over your performance.
Appointability
Raw interview score (RIS)
The RIS is the sum of all eight scores awarded to you during your interview, but before any weighting is applied.
As each individual score will be between 1 and 5, your RIS will be between 8 and 40.
Appointability requirements
To be classed as 'appointable', you must meet all three criteria below:
- none of your eight interview scores can be 1/5
- no more than two of your eight interview scores can be 2/5
- your RIS must be 24 or above.
If you meet all three requirements, your application will be assessed as appointable, and can progress to be considered for post offers.
However, if you fail to meet any of these requirements, your application must then be assessed as not appointable, and it will progress no further in that round.
Total score
After interview, a weighting is applied to the scores in each area, as well as your application score.
These scores are then combined to give your total score which determines your ranking, which will in turn be used to inform how offers are made. The weighting of different sections, as well as the method by which your total score is established, is detailed in the table accessible through the link below:
|
|
Interviewer 1
|
Interviewer 2
|
Weighting
|
Max score
|
|
Question 1 |
||||
|
Clinical scenario |
/ 5 |
/ 5 |
2.5 |
25 |
|
Question 2 |
||||
|
Professionalism & governance |
/ 5 |
/ 5 |
1.2 |
12 |
|
Question 3 |
||||
|
Presentation |
/ 5 |
/ 5 |
1.8 |
18 |
|
Question 4 |
||||
|
Suitability and commitment |
/ 5 | / 5 | 2.5 | 25 |
|
Raw interview score |
/ 40 |
|||
|
Interview score (w weighting) |
/ 80 |
|||
|
Application score |
/ 50 |
0.4 |
/ 20 |
|
|
Total score |
/ 100 |
|||
Indicative post numbers
Indicative vacancy numbers are available in the table below, broken down by region and divided between substantive national training number (NTN) and locum appointment for training (LAT) posts. In many cases these will be presented as a range (e.g. 1-4) as it is not always possible for regions to know at this stage how many vacancies there will be.
It is the intention that indicative post numbers for all regions will be published prior to the application opening date, although this cannot be guaranteed. Please note that this table is not likely to be updated subsequent to indicative numbers and actual numbers will be confirmed when programme preferences are opened later in the round.
Numbers subject to change
Please be aware that it is not uncommon for vacancy numbers to change as the round progresses.
More commonly, post vacancy numbers can increase as the round goes on (and confirmation of posts becomes available); but it is also possible that numbers can reduce as well. In the past, post numbers have risen an average of 20-40% from the start to the finish of the round but this can vary greatly for individual specialty/region combinations.
It is possible that regions which do not have a post at the start of the round may declare one after applications have closed. Whilst we try and minimise instances of this, it is not always possible to predict vacancies so even if there appears not to be a vacancy in your preferred specialty/region combination, you may wish to consider applying in case one becomes available during the round; you can check with the region concerned if you wish to check on the likelihood of a post arising.
Generally, once a region enter a post into a round they would always have at least one post available and would only withdraw it in exceptional circumstances.
Round 1 interview dates & posts
In this round, the specialties of allergy and immunology will hold a joint interview; whereby applicants to either specialty will undertake the same interview. Those applying to both will need only undertake one single interview.
| Region | NTN posts | LAT posts* | Evidence upload date(s) | Interview date(s) |
|---|---|---|---|---|
| East Midlands | 0 | N/A |
22/12/23 - 05/01/24 |
02/02/24 |
| East of England | 0 - 1 | N/A | ||
| London |
2 - 3 |
N/A | ||
| Kent, Surrey and Sussex | 0 | N/A | ||
| North East | TBC | N/A | ||
| North West |
0 - 1 |
N/A | ||
|
South West |
Peninsula |
N/A | ||
|
Severn |
N/A | |||
| Thames Valley | 0 | N/A | ||
| Wessex | 0 - 2 | N/A | ||
| West Midlands | 0 | N/A | ||
| Yorkshire & Humber | TBC | N/A | ||
| Scotland** | N/A | TBC | ||
| Wales | 0 | TBC |
*English LATs
Please note, English regions do not recruit to LAT posts.
**Scotland post numbers
If you are interested in working in Scotland, a breakdown of post numbers by the four Scottish regions is available on the Scottish Medical Training website. This has details of all specialty training post numbers in Scotland, including specialties which are not part of the nationally-coordinated process.
The SMT website will always be the more accurate one where they differ.
As part of the process of applying to HST, you may wish to gain an idea of how recruitment progressed in previous years for the various specialties participating in the nationally-coordinated recruitment.
To this end, we have published data dating back to 2013 (where this is available), based around four main areas:
-
Competition ratios - application numbers submitted to each specialty, along with the number of NTN and LAT posts available in each. It is worth noting that posts are subject to change throughout the round (increasing on average between 20-40%), and post numbers for this data are taken at the end of the round.
-
Shortlist scores - the scores awarded to all submitted applications, including average scores and distribution nationally.
-
Total scores - the total score awarded to all candidates who completed the full recruitment process for a specialty (application and interview), including some analysis of scores.
-
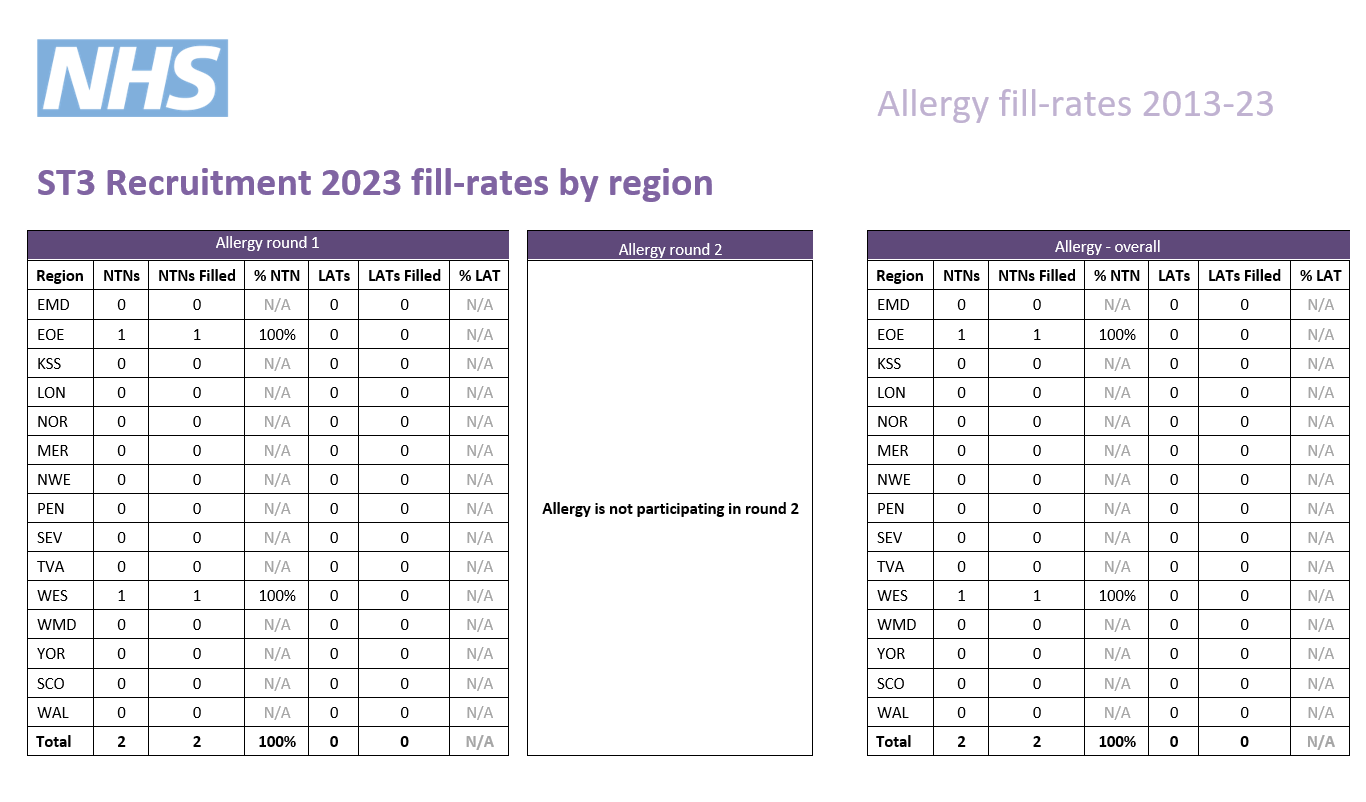
Post fill rates - the number of posts filled by region.
We have published information for all specialties participating in our process that year; consequently not all specialties will have data in all cases.
Round 1
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. | Unique* |
|---|---|---|---|---|---|---|
| 2023 | 35 | 2 | 0 | 2 | 17.5 | 6% |
| 2022 | 31 | 3 | 0 | 3 | 10.3 | 10% |
| 2021 | 21 | 4 | 0 | 4 | 5.3 | N/A* |
| 2020 | 11 | 3 | 0 | 3 | 3.7 | 18% |
| 2019 | 10 | 2 | 0 | 2 | 5.0 | 0% |
| 2018 | 11 | 1 | 0 | 1 | 11.0 | 27% |
| 2017 | 8 | 3 | 0 | 3 | 2.7 | 13% |
| 2016 | 7 | 1 | 0 | 1 | 7.0 | 43% |
| 2015 | 12 | 7 | 0 | 7 | 1.7 | 25% |
* the percentage of unique candidates that only applied to this specialty (out of the PSRO coordinated specialties)
** As many specialties did not participate in recruitment in 2021, the data is not comparable.
Round 2
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. |
|---|---|---|---|---|---|
| 2023 | Did not participate in round 2 | ||||
| 2022 | 17 | 1 | 0 | 1 | 17 |
| 2021 | 18 | 1 | 0 | 1 | 18 |
| 2020 | 16 | 3 | 0 | 3 | 5.3 |
| 2019 | Did not participate in round 2 | ||||
| 2018 | 3 | 1 | 0 | 1 | 3 |
| 2017 | 8 | 1 | 0 | 1 | 8 |
| 2016 | Did not participate in round 2 | ||||
| 2015 | 1 | 1 | 0 | 1 | 1 |