Training in an infection specialty is particularly interesting and varied because it combines both the clinical and laboratory skills of making diagnoses with the satisfaction of effective treatment for a wide range of common serious infections in both acutely and chronically ill patients.
There are four separate infection specialties: infectious diseases (ID), medical microbiology (MM), medical virology (MV) and tropical medicine (TM). To find out more about each of the specialties click on the pop-out boxes below.
Infectious diseases is a fascinating and rapidly changing specialty which offers the opportunity to see a wide range of patients, combine laboratory and clinical skills and spend time in research or working abroad in specialist centres. Particular challenges include the emergence of new diseases, and the increasing problems associated with antimicrobial resistance.
The training programme has recently been revised and all infection trainees will spend two years on a combined infection training (CIT) programme, with one year predominantly ID-based and one year spent attached to the microbiology laboratory and clinical consult rounds. This is followed by higher specialist training for a further three years in either ID/general medicine or ID/microbiology or ID/virology.
Infectious diseases involves in-patient work based in regional specialist ID Units, managing patients with a range of complex conditions including community acquired infections, returning travellers, TB, HIV, bone and joint infections and multi-drug resistant infections. Advice and consultation are provided for the management of nosocomial infections, antimicrobial stewardship and infections in immunocompromised patients.
Out-patient work includes travel-related conditions, tropical medicine and specialist clinics in HIV, TB, viral hepatitis and bone and joint infections. There is increasing use of out-patient antimicrobial therapy (OPAT) services.
The specialty will suit trainees who want to be challenged, who enjoy the interface between clinical and laboratory medicine and are keen on research. A large proportion of trainees go on to complete research projects leading to higher degrees and diplomas. Research and additional specialist experience is actively encouraged by the specialty advisory committee.
Medical microbiology is a varied and evolving specialty, involving all aspects of infection. It was formerly a very laboratory-based role, overseeing the diagnostic work, interpreting results and providing telephone advice to clinicians.
Increasingly it is more clinical and diverse, providing a rewarding mix of lab work, ward consults about cases of complex or serious infection, advising on how to control the spread of infection in hospitals and the community, infection-focused ward rounds and multidisciplinary meetings with many other specialties (including intensive care, haemato-oncology, orthopaedics), and the chance to take a lead role in developing new infection services such as OPAT (outpatient parenteral antibiotic treatment).
There is obvious overlap with infectious diseases, and it is possible to do dual training in both specialties; some centres have merged their microbiology and infectious diseases departments into combined departments of infection.
Clinical virology is an exciting specialty which is rarely out of the news and will appeal to those wishing to get involved in the interface between clinical work and research and development alongside an expanding clinical role.
The training programme provides an opportunity to be involved in a stimulating mix of clinical work, laboratory liaison, research, development and teaching. Clinical virologists concentrate on the diagnosis and management of patients with viral infections. Rapid diagnosis using molecular based tests, monitoring resistance to antiviral drugs, managing outbreaks of respiratory, gastrointestinal and other infections and learning the principles of laboratory diagnostic methods in a specialty that has always embraced new technologies are major parts of the job.
In addition, there is an opportunity to be involved in the management of patients with chronic viral infections such as HIV and hepatitis B and C, respiratory virus infections, congenital and perinatal infection and latent viral infections in immunocompromised patients, particularly transplant recipients.
In recent years, newly emerging virus infections have added to the breadth of interest and the skills required of the specialist virologist. Virology is important in the context of public health through input into surveillance and immunisation programmes. Laboratory and clinical research have traditionally been strong in this specialty; trainees wishing to obtain a higher degree will be actively encouraged.
For further information:
The Royal College of Pathologists, 6 Alie Street, London, E1 8QT
Phone: 020 7451 6700 Web: http://www.rcpath.org
UK Clinical Virology Network: http://www.clinicalvirology.org
There are a small number of training posts in tropical medicine, linked to either general internal medicine (entry at ST4), medical microbiology or medical virology (entry at ST3). The curriculum is similar to that for infectious diseases but differs in three ways:
- Trainees spend at least one year of their ID training at a recognised tropical centre in either Liverpool or London;
- An additional year of training must be spent working as a clinician at a recognised centre overseas; and
- Trainees must complete a face to face postgraduate qualification in tropical medicine such as the DTM&H.
Most tropical medicine specialists end up in academic positions, working abroad or overseeing collaborations between UK and international tropical centres. Research is actively encouraged.
Combined infection training (CIT)
The first two years, have a common combined infection training programme in all four specialties. After the two Combined Infection Training years the four specialties have their own separate higher specialty training programmes leading to a CCT in that particular specialty.
All four specialty training programmes include both clinical management of patients with infections and laboratory diagnostic experience. Most trainees undertake research leading to an MD or PhD degree at some point in training.
Infection training - trainee characteristics
Infection specialties will particularly suit trainees who enjoy:
-
a great variety of clinical presentations
-
the challenge of making the correct diagnosis
-
laboratory sciences.
Group 1 and Group 2 programmes
Recruitment to combined infection training programmes will be at ST4 and ST3 level, which means it contains both Group 1 and Group 2 specialty programmes. The 'Planning your application' tab has more information about how this affects applications to combined infection training as there are key differences compared to most specialties.
Joint specialty training
It's possible for two CCTs to be obtained as well as one CCT in an individual infection specialty. Joint programmes are available in a number of combinations and will require additional training time.
Initially, applcants will be in competition for all available posts across the infection specialties in the Group(s) to which they have applied. They will be able to preference their preferred CCT single specialty or joint specialties during the recruitment process. The available programme combinations are as follows:
Group 1
- Infectious diseases and general internal medicine
- Tropical medicine and general internal medicine
Group 2
- Infectious diseases and medical microbiology
- Infectious diseases and medical virology
- Medical microbiology
- Medical virology
- Tropical medicine and medical microbiology
- Tropical medicine and medical virology
Working/training in an infection specialty training post
Training in the infection specialties is particularly interesting and unlike many medical specialties infection specialties are not confined to a single organ or system. Infections can present in many different ways, in patients of all ages and backgrounds. Combined infection training offers a broad training in the diversity of infection diagnosis and management in a range of clinical settings, both outside and inside the infectious diseases unit, and includes time learning laboratory skills and antimicrobial and infection control management.
Diagnostical skill
Making the correct diagnosis often involves considerable detective skill in history-taking, physical examination and interpretation of laboratory data.
Treating serious infections in acutely ill patients is very satisfying, because the vast majority of patients make an excellent recovery, and this is increasingly true for many patients with chronic infections.
Before entering higher specialty training, core experience in a broad range of specialties is desirable; prior experience of any of the infection specialties is useful but not essential.
Career prospects
Many infection specialty consultants work in teaching hospitals with access to specialised investigations and many pursue research interests.
The increasing number of infection related consultant posts is evidence of the wider recognition of the distinctive clinical value of the various infection disciplines.
Given the growing numbers of patients with HIV and tuberculosis, the widespread use of immuno-suppressive treatments, increasing transplantation numbers, breakthroughs in hepatitis management, and the importance of healthcare-associated infections and management of antimicrobial prescribing, there has never been a better time to become an infection specialist. Changes in laboratory practice have meant that medical virologists and microbiologists not only have access to increasingly sophisticated diagnostics but also have clinical roles alongside infectious diseases and tropical medicine colleagues.
Further information
General/application queries
For general queries relating to areas such as eligibility criteria, making an application or the Oriel system, please contact the Physician Specialty Recruitment Office.
Queries regarding the progress of a submitted application should be directed to the lead recruiter for this specialty. The lead recruiter for combined infection training is Scotland. If your query is related to 2022 R2 recruitment, please contact Thames Valley [email protected]
| NHS Education for Scotland | ||||||
|---|---|---|---|---|---|---|
| General queries* | [email protected] | |||||
Group 1 and Group 2 programmes included
Recruitment to combined infection training programmes will be at ST4 and ST3 level, which means it contains both Group 1 and Group 2 specialty programmes. Those wishing to apply need to be aware of how this impacts the process and what you will need to do, as there are key differences compared to most specialties.
- Group 1 – this includes infectious diseases, and tropical medicine where available, programmes which are dual accredited with general internal medicine. It is not possible to single accredit in infectious diseases and tropical medicine.
- Group 2 – this includes:
- Single accredited programmes in medical microbiology or medical virology
- Infectious diseases or tropical medicine programmes which are dual accredited with either medical microbiology or medical virology.
Two vacancies/applications, one interview
There will be two combined infection training vacancies, one at ST3 and one at ST4. If you are eligible, and wish to be considered, for both ST3 and ST4 programmes, you will need to submit two applications – one to each vacancy. Those applying to, and eligible for, both vacancies will undergo a single interview, with scores used for both vacancies; more detail is included further down the page and on the ‘Interview & scoring’ tab in this section.
Eligibility
Combined infection training only accepts candidates from physician training routes. However, Group 1 and Group 2 specialties have differing entry requirements:
- Group 1 – eligibility requires completion of the internal medicine training (IMT) stage 1 programme or equivalent.
- Group 2 – eligibility requires completion of the first two years of the internal medicine training (IMT) stage 1 programme or equivalent.
If you are eligible for Group 1 programmes, you will, by default, be eligible for Group 2. Please visit the am I eligible? section of this website for further information about the eligibility criteria for both Group 1 and Group 2 specialties.
Commitment to specialty
Combined infection training will be assessing your commitment to specialty as part of the shortlisting process. This will be looking at your commitment to infection training and will be scored based on your activity and interest across any of the specialties included in the combined infection training programme. Please visit the application scoring page for general information about how this is assessed and scored.
How applying to both vacancies will work
The information below is advice for those planning to apply to both vacancies.
Applying
The two vacancies will have identical application forms and it will be necessary to duplicate the information across both. If you completely submit one application before starting the other, you will be given opportunity to request some sections of the form are copied over but will have to manually copy over the ‘Evidence’ and ‘Supporting’ sections. There is no need to tailor the application form for the two different vacancies and you should directly copy between the two.
Evidence verification and shortlisting
Your application will be assessed once, with scores copied to both vacancies; you will only need to upload evidence once. Shortlisting will either be for both vacancies or neither, you will not be shortlisted for one and not the other.
Invitations to interview
It is anticipated that applicants to this specialty will be allocated to their interview slot and there will not be opportunity to self-book as happens with other specialties. This is because it needs to be managed when those just in contention for ST3 and those in contention for ST4 are interviewed due to the different length of interview and the make-up of the interviewers needed. It will be confirmed nearer the time if the situation is any different to this.
Interview and ranking
You will attend a single interview with an additional Group 1 medical registrar suitability question in an additional station for those in contention for ST4 vacancies. You could be found appointable for Group 2 but not Group 1 if your performance in the medical registrar suitability question means you do not meet the ST4 criteria. If you have been found not appointable for ST3, you cannot be considered appointable for ST4, even if your score in the medical registrar suitability question enables you to meet the ST4 criteria.
Interview scores will be duplicated across both vacancies, with the additional question scores added for the ST4 application. This means you will get two independent final assessment scores and rankings, ranked against the other applicants within each vacancy.
The ‘Interview & scoring’ gives further details on these areas.
Preferences and offers
You will need to separately preference the programmes within each vacancy as there will be a separate offers process for Group 1 and Group 2 so, depending on your rank and preferences, you may receive two offers. You can hold one whilst awaiting the outcome of the other, as per the normal offer rules.
As part of the process of applying to HST, you may wish to gain an idea of how recruitment progressed in previous years for the various specialties participating in the nationally-coordinated recruitment.
To this end, we have published data dating back to 2013 (where this is available), based around four main areas:
-
Competition ratios - application numbers submitted to each specialty, along with the number of NTN and LAT posts available in each. It is worth noting that posts are subject to change throughout the round (increasing on average between 20-40%), and post numbers for this data are taken at the end of the round.
-
Shortlist scores - the scores awarded to all submitted applications, including average scores and distribution nationally.
-
Total scores - the total score awarded to all candidates who completed the full recruitment process for a specialty (application and interview), including some analysis of scores.
-
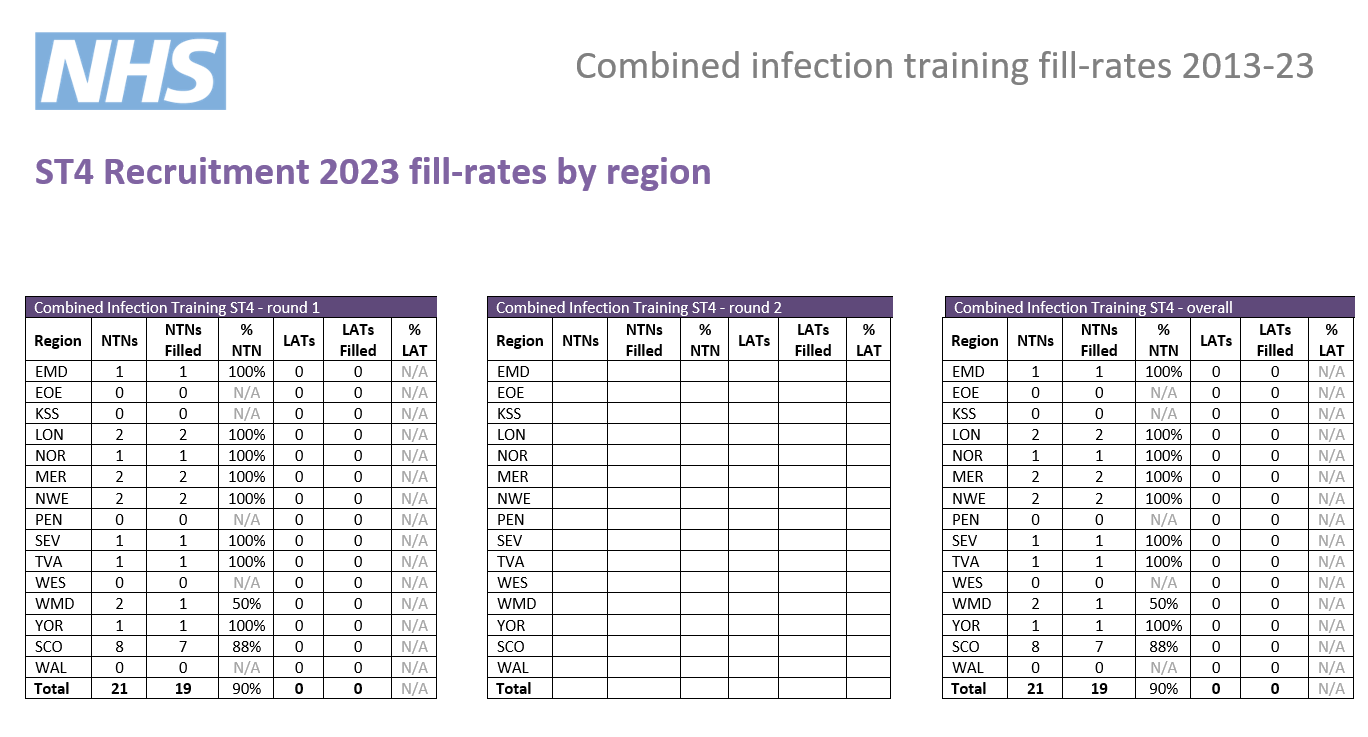
Post fill rates - the number of posts filled by region.
We have published information for all specialties participating in our process that year; consequently not all specialties will have data in all cases.
Round 1
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. | Unique* |
|---|---|---|---|---|---|---|
|
2023 |
ST4 - 88 | 21 | 0 | 21 | 4.2 | 7% |
| ST3 - 160 | 40 | 0 | 40 | 4 | 43% | |
|
2022 |
ST4 - 113 | 24 | 0 | 24 | 4.7 | 8% |
| ST3 - 162 | 33 | 1 | 34 | 4.8 | 35% | |
| 2021 | 170 | 53 | 0 | 53 | 3.2 | N/A** |
| 2020 | 197 | 54 | 0 | 54 | 3.6 | 57% |
| 2019 | 136 | 63 | 0 | 63 | 2.2 | 69% |
| 2018 | 125 | 70 | 0 | 70 | 1.8 | 65% |
| 2017 | 104 | 53 | 0 | 53 | 2.0 | 67% |
| 2016 | 97 | 56 | 0 | 56 | 1.7 | 63% |
| 2015 | 97 | 62 | 10 | 72 | 1.3 | 54% |
* the percentage of unique candidates that only applied to this specialty (out of the PSRO-coordinated specialties)
** As many specialties did not participate in recruitment in 2021, the data is not comparable.
Round 2
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. |
|---|---|---|---|---|---|
| 2023 | ST4 - | ||||
| ST3 - | |||||
| 2022 | ST4 - 32 | 5 | 0 | 5 | 6.4 |
| ST3 - 54 | 20 | 0 | 20 | 2.7 | |
| 2021 | 85 | 20 | 0 | 20 | 4.2 |
| 2020 | 130 | 17 | 0 | 17 | 7.6 |
| 2019 | 61 | 32 | 0 | 32 | 1.9 |
| 2018 | 40 | 35 | 0 | 35 | 1.1 |
| 2017 | 36 | 28 | 0 | 28 | 1.3 |
| 2016 | 25 | 19 | 0 | 19 | 1.3 |
| 2015 | 17 | 22 | 7 | 29 | 0.6 |
Indicative post numbers
Indicative vacancy numbers are available in the table below, broken down by region and divided between substantive national training number (NTN) and locum appointment for training (LAT) posts. In many cases these will be presented as a range (e.g. 1-4) as it is not always possible for regions to know at this stage how many vacancies there will be.
It is the intention that indicative post numbers for all regions will be published prior to the application opening date, although this cannot be guaranteed. Please note that this table is not likely to be updated subsequent to indicative numbers and actual numbers will be confirmed when programme preferences are opened later in the round.
Numbers subject to change
Please be aware that it is not uncommon for vacancy numbers to change as the round progresses.
More commonly, post vacancy numbers can increase as the round goes on (and confirmation of posts becomes available); but it is also possible that numbers can reduce as well. In the past, post numbers have risen an average of 20-40% from the start to the finish of the round but this can vary greatly for individual specialty/region combinations.
It is possible that regions which do not have a post at the start of the round may declare one after applications have closed. Whilst we try and minimise instances of this, it is not always possible to predict vacancies so even if there appears not to be a vacancy in your preferred specialty/region combination, you may wish to consider applying in case one becomes available during the round; you can check with the region concerned if you wish to check on the likelihood of a post arising.
Generally, once a region enter a post into a round they would always have at least one post available and would only withdraw it in exceptional circumstances.
Round 1 Interview dates & posts
Available infection specialty combinations will be listed in brackets where known.
| Region | ST3 NTN posts | ST4 NTN posts | LAT posts* | Evidence upload date(s) | Interview date(s) |
|---|---|---|---|---|---|
| East Midlands |
1 ID/MM |
1 |
N/A |
22/12/23 - 05/01/24 |
25, 26, 27, 28 March 2024 |
| East of England |
0 - 9 |
0-1 |
N/A |
||
|
London |
0 - 2 ID/MM 0 - 2 ID/V |
0 - 1 |
N/A |
||
|
Kent, Surrey and Sussex |
0 - 2 ID/MM 0 - 2 ID/V
|
0 - 2 |
N/A |
||
| North East |
0 - 2 |
0 - 1 |
N/A |
||
|
North West |
Mersey 0 - 1 ID/MM 0 - 1 ID/MV |
Mersey 0 - 1 |
N/A |
||
|
North West 0 - 3 ID/MM 0 - 3 ID/MV |
North West 0 - 3 |
N/A |
|||
| South West |
Peninsula 0 - 1 |
0 |
N/A |
||
|
Severn 0 - 1 CIT/ID/MM |
0 - 1 |
N/A |
|||
| Thames Valley |
0 - 2 ID/MM |
0 - 1 |
N/A |
||
| Wessex |
0 - 2 MM/ID |
0 - 1 |
N/A |
||
| West Midlands |
1 - 2 ID/MM |
0 - 1 |
N/A |
||
| Yorkshire & Humber |
0 |
0 |
N/A |
||
| Scotland** |
1 - 2 ID/MM |
1-2 |
TBC |
||
| Wales |
1 - 2 |
0 |
TBC |
*English LATs
Please note, English regions do not recruit to LAT posts.
**Scotland post numbers
If you are interested in working in Scotland, a breakdown of post numbers by the four Scottish regions is available on the Scottish Medical Training website. This has details of all specialty training post numbers in Scotland, including specialties which are not part of the nationally-coordinated process.
The SMT website will always be the more accurate one where they differ.
Interview content
There is a slightly different interview depending on whether you are in contention for Group 1 programmes or just Group 2. There will be two stations for group 2 and three stations for group 1. There are four questions for Group 2 candidates in this interview, ranging between 4 - 6 minutes in length, and the additional 'Medical registrar suitability' question for Group 1 candidates lasting ten minutes.
Each station will last 10 minutes, so including the time between stations, the interview will be approximately 30 minutes for group 2 and 45 for group 1.
Please note that this is subject to change and will be confirmed by the date of interview.
For this question you will be asked to give a presentation, which you are expected to prepare in advance on a given subject (see below). This will be followed by discussion of your presentation between you and the interviewers.
Presentation
You will need to give a presentation on the following topic, for no more than three minutes:
'An interesting recent development / research finding, relevant to infection specialties (including infectious diseases, medical microbiology, medical virology or tropical medicine)'
When preparing your presentation, please bear in mind the points below:
- Clarity & relevance most important - Select a topic that is relevant to infection specialties, and which you can present with clarity. This is more important than trying to impress by choosing a subject that is esoteric or complex. It should be relevant to your application where possible.
- Three-minute time limit - Your presentation must last for no more than three minutes. Please note that you will be stopped after three minutes so as to allow further discussion to take place, so try and get your main points across before then. At the same time, bear in mind that interviewers will be assessing the level, depth and content of your presentation, as well as expecting some structure.
-
No aids/resources allowed – you are not allowed to use any visual representations, such as PowerPoint, when giving your presentation and you must not share your screen. You are welcome to use prompts on small cards, but these should be for your own use only.
Interview nerves will also be taken into consideration.
Post-presentation discussion
Once your presentation is finished (interviewers will stop you at the three minute-mark), interviewers will discuss it with you and ask further questions relating to the items you raise and any further points.
This discussion will take place for approximately 3 minutes.
This question will focus on your suitability for and commitment to HST training in the specialty and give you opportunity to expand on the information provided in your application form.
This question will last approximately 4 minutes.
Prior to question 3 you will be given a clinical scenario to review; you will have a short while to review the scenario. You will then have approximately 6 minutes where the panel will ask you questions regarding the scenario.
The clinical scenario will be relatively brief (two/three sentences), so once you have read this, the remainder of the reading time will allow you to undertake some short preparation (just mental preparation - this does not mean making notes, etc.)
Scenario considerations
The scenario will describe a hypothetical clinical situation which has arisen in which you are, or have become, involved. Some points to consider when reviewing the scenario and preparing for discussion are:
- what steps you would take
- any potential treatments possible
- any further information you would gather
- how you would go about communicating with any people (eg patients, family members, colleagues) involved in the scenario.
You should take into account any other factors you deem appropriate, using your experience and professional judgement.
You will be asked a question which focuses on one or more of these areas. This question will not be available to you to consider in advance and the hypothetical scenario will be given on completion of the clinical scenario.
This question will not focus on clinical aspects, and will deal with the moral, ethical, legal, etc. issues of a particular situation. Your answer should be guided by GMC Good Medical Practice.
This question will last up to 4 minutes.
This question will explore the non-clinical aspects of being a medical registrar, focusing on two of the Capabilities in Practice (CiPs) from the Internal Medicine Stage 1 Curriculum:
- Managing an acute unselected take
- Managing a multi-disciplinary team including effective discharge planning
This discussion will be prompted by a short question provided by interviewers. This will not be given to you before - this will be given verbally by interviewers once the previous question is finished. This question will last approximately 10 minutes.
Questioning will ask you to draw on your experience of managing a team caring for acute medical admissions by giving examples of how you have managed that type of situation.
Scoring framework
The score of 1-5 an interviewer will award you for each assessment area is judged in relation to how well you perform against an expected level. Below is the framework used to award scores at interview, as well as interpretation of what these scores represent:
|
Mark
|
Rating
|
Assessment
|
|
1 |
poor |
not considered appointable |
|
2 |
area for concern |
performed below the level expected from a core level trainee applying to the specialty; |
|
3 |
satisfactory |
performed at the level expected of a core level trainee applying to the specialty; |
|
4 |
good |
above average ability; |
|
5 |
excellent |
highly performing trainee; |
As shown in the table, for each of the question areas at interview, 3/5 is considered a satisfactory score; and reflects the level of performance that would be expected of a trainee ready to progress to a specialty training programme.
Should your performance go above and beyond this expected level, interviewers can award marks of 4/5 or 5/5 as appropriate.
Conversely, should your interview performance not reach the expected level, then interviewers can award marks of 1/5 or 2/5, as reflects their level of concern over your performance.
Appointability
The appointability requirements differ slightly for the Group 1 and Group 2 assessments.
Group 1
Raw interview score
The RIS is the sum of all ten scores awarded to you during your interview, but before any weighting is applied.
As each individual score will be between 1 and 5, your RIS will be between 10 and 50.
Appointability requirements
To be classed as 'appointable', you must meet all the criteria below:
- none of your ten interview scores can be 1/5
- no more than two of your ten interview scores can be 2/5
- your RIS must be 30 or above
- you must also meet the criteria for the Group 2 assessment, i.e. discounting the medical registrar suitability question; whilst it is possible to be considered for appointment for ST3 but not ST4, it is not possible the other way round.
If you meet all these requirements, your application will be assessed as appointable, and can progress to be considered for offers.
However, if you fail to meet any of these requirements, your application must then be assessed as not appointable, and it will progress no further in that round.
Group 2
Raw interview score
The RIS is the sum of all eight scores awarded to you during your interview, but before any weighting is applied.
As each individual score will be between 1 and 5, your RIS will be between 8 and 40.
Appointability requirements
To be classed as 'appointable', you must meet all three criteria below:
- none of your eight interview scores can be 1/5
- no more than two of your eight interview scores can be 2/5
- your RIS must be 24 or above.
If you meet all three requirements, your application will be assessed as appointable, and can progress to be considered for post offers.
However, if you fail to meet any of these requirements, your application must then be assessed as not appointable, and it will progress no further in that round.
Total score
After interview, a weighting is applied to the scores in each area, as well as your application score.
These scores are then combined to give your total score which determines your ranking, which will in turn be used to inform how offers are made. The weighting of different sections, as well as the method by which your total score is established, is detailed in the table below:
|
|
Interviewer 1
|
Interviewer 2
|
Weighting
|
Max score
|
|
Question 1 |
||||
|
Presentation |
/ 5 |
/ 5 |
ST3 - 2.5 ST4 - 2.0 |
25 20 |
|
Question 2 |
||||
|
Suitability & commitment |
/ 5 |
/ 5 |
ST3 - 1.8 ST4 - 1.5 |
18 15 |
|
Question 3 |
||||
|
Clinical scenario |
/ 5 |
/ 5 |
ST3 - 2.5 ST4 - 2.0 |
25 20 |
|
Question 4 |
|
|||
|
Ethical, professionalism and governance |
/ 5 |
/ 5 |
ST3 - 1.2 ST4 - 1.5 |
12 15 |
|
Question 5 (Group 1 only) |
||||
| Medical registrar suitability | / 5 | / 5 | 1 | 10 |
| Application score | / 50 | 0.4 | / 20 | |
| Group 1 | Group 2 | |||
| Raw interview score | / 50 | / 40 | ||
|
Interview score (w weighting) |
/ 80 |
/ 80 |
||
|
Total score |
/ 100 |
/ 100 |
||