From August 2022, all genitourinary medicine higher specialty trainees will dual accredit in Genitourinary Medicine and Internal Medicine. This will be delivered in a blended approach to allow trainees to maintain and develop their skills in internal medicine, whilst becoming an expert in genitourinary and HIV medicine.
Genitourinary Medicine (GUM) is one of the most diverse, unique and advancing specialities, covering the prevention and management of sexually transmitted infections and HIV, and so much more.
As a GUM trainee (and consultant) you can:
- diagnose and treat conditions on the same day to managing long term chronic conditions;
- take an active role in public health;
- look after the cycle of life from adolescents to pregnant women and older patients;
- specialise in various areas including psychosexual medicine, contraception, chronic genital problems including infections and dermatological conditions within sexual health;
- manage the complexities HIV brings including opportunistic infections, HIV related and non-HIV related co-morbidities, antiretroviral drug resistance, adherence issues, largely in the outpatient setting but also inpatient setting;
- manage key and vulnerable populations including young, sex workers and drug users, refugees, etc.
Specialising in GUM not only provides the opportunity to work within a diverse multi-disciplinary team from specialist nurses, specialist pharmacists, health advisors, psychologists to peer support workers on a daily basis, but a diverse patient population group making communication skills, a non-judgemental attitude and empathetic nature ingrained for GUM physicians.
Trainees are actively encouraged and supported throughout their training to undertake opportunities and develop in their career towards a consultant GUM physician. Out of programme experiences have included stints abroad in Africa, Asia, Middle East and Europe, training as sexual offences examiner, Public Health England fellowships, and furthering education qualifications, to name a few. Academic experiences are fostered through general training including service evaluation through QUIPS and audits, but formally through academic posts, with local, national and international collaborations always available. Strong links exists for trainees within the work of the British Association for Sexual Health and HIV, British HIV Association extending to a number of international organisations. As a consultant, it is easy to continue those interests above and beyond.
Above all, GUM is a fun speciality, that will not only satisfy the clinical and psycho-social aspects of medicine from a generalist and specialist perspective, but provides a whole array of other opportunities while still being able to maintain a healthy work life balance!
“One of the best things for me about working in GUM is that I really enjoy going to work every day; not many of my friends say that about their jobs in other careers." GUM trainee.
GUM - trainee characteristics
The nature of genitourinary medicine requires trainees who are:-
non-judgemental
-
excellent communicators
-
team players
- adaptability, given the evolving nature of the specialty
-
not easily embarrassed, with a good sense of humour!
Working/training in an HST GUM post
The day-to-day work of a GUM physician varies, depending on sub-specialty and setting, and ranges from managing acute presentations of STIs, sexual assault assessment and post-exposure prophylaxis for HIV in addition to routine reproductive and sexual healthcare provision and the longterm management of chronic HIV infection.
There are also more specialist services, such as psychosexual medicine, adolescent clinics and genital dermatology, as well as sex worker and drug user outreach services.
Emphasis on social factors and community-based care
As many of our patients are drawn from vulnerable and under-represented populations, there is also a real emphasis on social circumstances and emotional health.
Traditionally, GUM clinics were based in hospital; however these are becoming increasingly community-based, so as to provide better local access, although HIV care has continued in acute settings.
Inter-disciplinary work and work-life balance
The specialty provides ample opportunity for interdisciplinary working with sexual and reproductive health, infectious diseases, diagnostics specialties and public health; the latter being a key element of the specialty with regards to partner notification and disease surveillance.
GUM physicians work alongside the ever-increasing multidisciplinary team, including professionals of various disciplines - primarily nurses, health advisers, general practitioners, pharmacists, school nurses and other allied professionals.
GUM is predominantly an out-patient specialty with limited on-call. Dual accreditation in GUM and internal medicine will enable trainees to consider employment in a variety of settings including acute medicine, community hubs or in specialist sexual health work, such as sexual assault referral centres and outreach clinics.
Trainee satisfaction
GUM has achieved high scores for satisfaction in the annual GMC trainee survey, and most trainees feel prepared for consultant posts after the four-year training programme.
The GMC accepted the revised GUM curriculum in 2021 and it will be implemented from August 2022. The curriculum is delivered through a variety of learning experiences, including work-based learning and on-the-job supervision.
Out-of-programme attachments have been encouraged, and a number of trainees pursue HIV care abroad or higher degrees.
A day in the life of an ST5 GUM registrar...
To give an indication of what you can expect from time in a GUM post, we asked an ST5 trainee to describe a common day for them.
Morning meeting
Today is Monday so I start with our HIV multidisciplinary meeting at 9am in our HIV hospital base.
This multidisciplinary meeting is attended by the GUM consultants, registrars, specialist nurses, sexual health advisers, virologists, psychiatrists and counsellors, as well as some cakes or biscuits!
We review each of the patients coming to clinic over the next week and discuss difficult management or, more often than not, challenging social circumstances.
Clinic
Clinic starts later in the morning and my first patient is indeed a challenge - a newly diagnosed lady from Africa who has been trafficked to the UK and does not speak any English.
The consultation is challenging, especially with a translator; however, after an hour or so we make some progress and link her in with social work, TARA and the red cross.
My next patient is a gentleman who wishes to start a family with his HIV-negative wife. We discuss all the options and make a referral for fertility assessment.
After this I see a patient who has not attended for three years. He's short of breath with oral candida, so I arrange admission to our ward for further assessment with just enough time to make our STI diagnostics group meeting.
Diagnostics group
This group is attended by public health and virology colleagues to review local STI trends and new diagnostic tests, and attending really helps in appreciating the GUM specialty as a whole.
Community sexual health clinic
In the afternoon I'm based in one of our community hubs with two specialist nurses for the sexual health clinic.
As our service is fully integrated, the afternoon is as varied as always, including gonorrhoea-diagnosed by onsite microscopy, emergency IUD fitting, PEP for HIV after a condom break, post-menopausal bleeding as well as a prolonged discussion with the partner of a patient recently diagnosed with herpes simplex.
Young persons clinic
Later in the day the young persons clinic starts with its usual added complexities. I see a 14-year-old with a history of liver transplant for contraception advice, as well as a group of 12-year-old boys asking for condoms with the usual jokes and giggles...
At the end of the clinic I see a vulnerable 12-year-old girl who discloses her excessive drinking and sexual contact, at which point I discuss her case with our specialist young persons consultant, and subsequently social work.
End of the day...almost
My normal day is supposed to finish here, at 5pm; however, I also participate in our Sexual Assault Referral Centre on-calls, and today I am on call from 5pm till 9am the next morning. I just hope it's a quiet night!
Further information
General / application queries
For general queries relating to areas such as eligibility criteria, making an application or the Oriel system, please contact the Physician Specialty Recruitment Office.
Queries regarding the progress of a submitted application should be directed to the lead recruiter for this specialty. The lead recruiter for genitourinary medicine is East Midlands.
| NHS England East Midlands | ||||||
|---|---|---|---|---|---|---|
| Postal address | East Midlands Westbridge Place 1 Westbridge Close Leicester LE3 5DR |
|||||
| email address 1 (ST4/general queries) | [email protected] | |||||
| email address 2 (fitness to practise queries - confidential) | ||||||
| website | https://www.eastmidlandsdeanery.nhs.uk/ | |||||
Group 1 specialty
This is a Group 1 specialty and requires completion of the internal medicine training (IMT) stage 1 programme or equivalent; all programmes in the specialty will dual specialise with general internal medicine.
Therefore, this specialty uses the standard HST eligibility criteria for Group 1 specialties and does not accept candidates from any alternative training routes. Please visit the am I eligible? section of this website for further information.
Commitment to specialty
The specialty will not be assessing your commitment to specialty as part of the shortlisting process and will score your application purely via the self-assessment scoring framework. Commitment to specialty will be assessed as part of the interview.
As part of the process of applying to HST, you may wish to gain an idea of how recruitment progressed in previous years for the various specialties participating in the nationally-coordinated recruitment.
To this end, we have published data dating back to 2013 (where this is available), based around four main areas:
-
Competition ratios - application numbers submitted to each specialty, along with the number of NTN and LAT posts available in each. It is worth noting that posts are subject to change throughout the round (increasing on average between 20-40%), and post numbers for this data are taken at the end of the round.
-
Shortlist scores - the scores awarded to all submitted applications, including average scores and distribution nationally.
-
Total scores - the total score awarded to all candidates who completed the full recruitment process for a specialty (application and interview), including some analysis of scores.
-
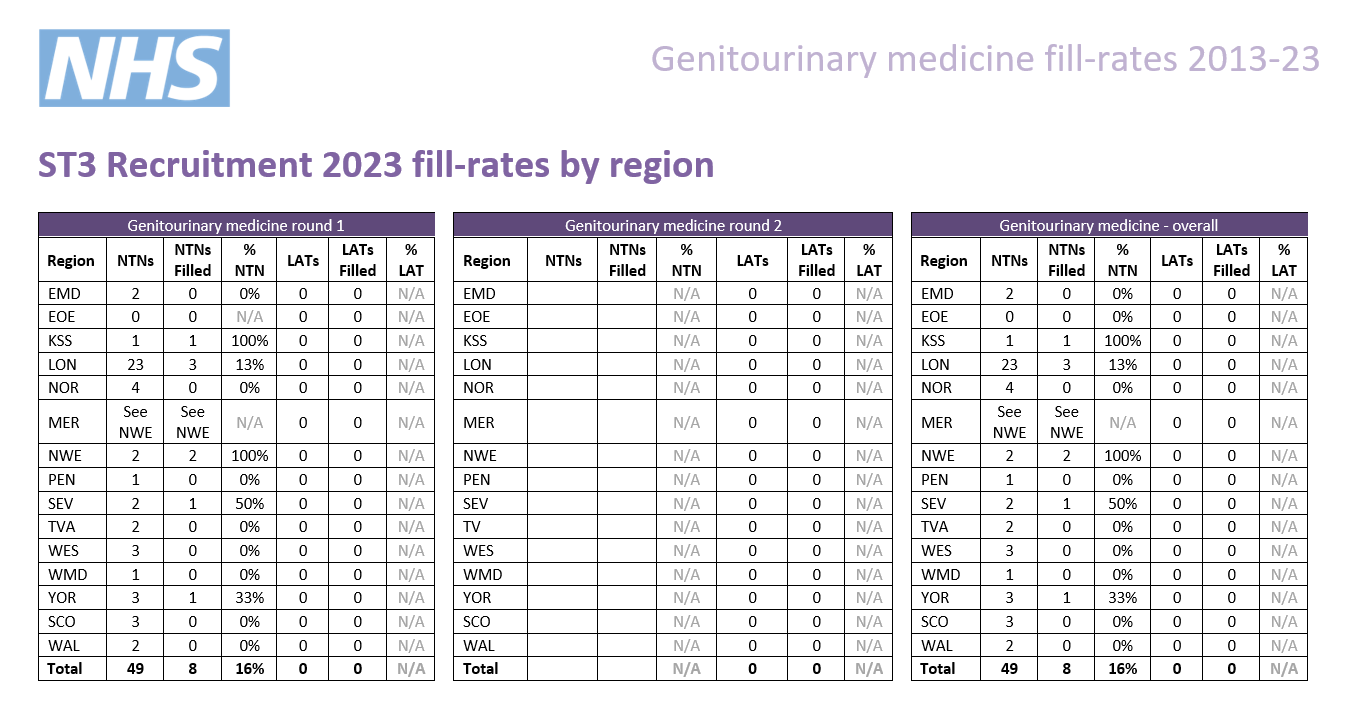
Post fill rates - the number of posts filled by region.
We have published information for all specialties participating in our process that year; consequently not all specialties will have data in all cases.
Round 1
| Year | Apps. | NTN posts | LAT posts | Total posts | Comp. | Unique* |
|---|---|---|---|---|---|---|
| 2023 | 23 | 49 | 0 | 49 | 0.5 | 30% |
| 2022 | 17 | 35 | 0 | 35 | 0.5 | 18% |
| 2021 | 30 | 38 | 0 | 38 | 0.7 | N/A** |
| 2020 | 30 | 53 | 0 | 53 | 0.6 | 27% |
| 2019 | 20 | 46 | 0 | 46 | 0.4 | 70% |
| 2018 | 22 | 37 | 0 | 37 | 0.6 | 59% |
| 2017 | 38 | 33 | 0 | 33 | 1.2 | 45% |
| 2016 | 34 | 35 | 0 | 35 | 0.9 | 47% |
| 2015 | 35 | 29 | 15 | 44 | 0.8 | 60% |
* the percentage of unique candidates that only applied to this specialty (out of the PSRO-coordinated specialties)
** As many specialties did not participate in recruitment in 2021, the data is not comparable.
Round 2
| Year | Apps. | NTN posts | LAT posts | Total posts | Comps. |
|---|---|---|---|---|---|
| 2023 | |||||
| 2022 | 3 | 29 | 0 | 29 | 0.1 |
| 2021 | 19 | 34 | 0 | 34 | 0.5 |
| 2020 | 28 | 34 | 0 | 34 | 0.8 |
| 2019 | This specialty did not take part in round 2 | ||||
| 2018 | 1 | 0 | 0 | 0 | 0 |
| 2017 | 7 | 21 | 0 | 21 | 0.3 |
| 2016 | 8 | 17 | 0 | 17 | 0.5 |
| 2015 | 7 | 21 | 8 | 29 | 0.2 |
Indicative post numbers
Indicative vacancy numbers are available in the table below, broken down by region and divided between substantive national training number (NTN) and locum appointment for training (LAT) posts. In many cases these will be presented as a range (e.g. 1-4) as it is not always possible for regions to know at this stage how many vacancies there will be.
It is the intention that indicative post numbers for all regions will be published prior to the application opening date, although this cannot be guaranteed. Please note that this table is not likely to be updated subsequent to indicative numbers and actual numbers will be confirmed when programme preferences are opened later in the round.
Numbers subject to change
Please be aware that it is not uncommon for vacancy numbers to change as the round progresses.
More commonly, post vacancy numbers can increase as the round goes on (and confirmation of posts becomes available); but it is also possible that numbers can reduce as well. In the past, post numbers have risen an average of 20-40% from the start to the finish of the round but this can vary greatly for individual specialty/region combinations.
It is possible that regions which do not have a post at the start of the round may declare one after applications have closed. Whilst we try and minimise instances of this, it is not always possible to predict vacancies so even if there appears not to be a vacancy in your preferred specialty/region combination, you may wish to consider applying in case one becomes available during the round; you can check with the region concerned if you wish to check on the likelihood of a post arising.
Generally, once a region enter a post into a round they would always have at least one post available and would only withdraw it in exceptional circumstances.
Round 1 Interview dates & posts
| Region | NTN posts | LAT posts* | Evidence upload date(s) | Interview date(s) |
|---|---|---|---|---|
| East Midlands | 3 | N/A |
09/01/24 - 16/01/24 |
06/03/24 |
|
East of England |
0 - 2 | N/A | ||
|
London |
10 - 53 |
N/A | ||
|
Kent, Surrey and Sussex |
0 - 3 |
N/A | ||
| North East | 0 - 4 | N/A | ||
| North West |
0 - 1 |
N/A | ||
|
South West |
Peninsula 0 - 2 |
N/A | ||
|
Severn 0 - 1 |
N/A | |||
| Thames Valley | 1 - 2 | N/A | ||
| Wessex | 1 - 3 | N/A | ||
| West Midlands | 1 - 2 | N/A | ||
| Yorkshire & Humber | 0 - 1 | N/A | ||
| Scotland** |
5 |
TBC | ||
| Wales | 2 | TBC |
*English LATs
Please note, English regions do not recruit to LAT posts.
**Scotland post numbers
If you are interested in working in Scotland, a breakdown of post numbers by the four Scottish regions is available on the Scottish Medical Training website. This has details of all specialty training post numbers in Scotland, including specialties which are not part of the nationally-coordinated process.
The SMT website will always be the more accurate one where they differ.
Interview content
The interview will be split across two separate stations with a separate pair of interviewers scoring you on the areas within their station. There will be four questions of 10 minutes in length. You will be marked on these questions and your communication skills, giving five scored areas in total. The headings below show the question areas and in which station they will be covered, along with information about what will be assessed.
Each station will last 20 minutes, so including the time between stations, the interview will be approximately 50 minutes.
Please note that this is subject to change, and will be confirmed by the date of interview.
Prior to this question you will be given a clinical scenario and a short while to review it. You will then be asked questions relating to this scenario. Your communication skills will also be assessed during this question and marked accordingly. This question will last approximately 10 minutes.
The clinical scenario will be relatively brief (two/three sentences), so once you have seen this, the remainder of the preparation time will allow you to undertake some short mental preparation. Whilst it is permitted to make notes, these must be destroyed as soon as your interview is completed and not shared with anyone.
Clinical scenario considerations
The scenario will describe a hypothetical clinical situation which has arisen in which you are, or have become, involved. Some points to consider when reviewing the scenario and preparing for discussion are:
- what steps you would take
- any potential treatments possible
- any further information you would gather
- how you would go about communicating with any people (eg patients, family members, colleagues) involved in the scenario
You should also consider any other factors you deem appropriate, using your experience and professional judgement.
Areas for assessment
One mark will be awarded to you based on your suggestions and responses to the clinical scenario. The second mark will be on the communication skills you display.
This will be both an assessment of how you would communicate with patients, colleagues, etc. in the scenario, as well as of how well you communicate with interviewers.
This question will explore the non-clinical aspects of being a medical registrar, focusing on two of the Capabilities in Practice (CiPs) from the Internal Medicine Stage 1 Curriculum:
- Managing an acute unselected take
- Managing a multi-disciplinary team including effective discharge planning
This discussion will be prompted by a short question provided by interviewers. This will not be given to you before - this will be given verbally by interviewers once the previous question is finished. This question will last approximately 10 minutes.
Questioning will ask you to draw on your experience of managing a team caring for acute medical admissions by giving examples of how you have managed that type of situation.
This question will see you given an ethical scenario to review. As with the clinical scenario in question 1, this ethical scenario takes the form of a hypothetical situation, described briefly in text form, details of which will be given to you before answering the question. You will have a short while to review the scenario and there will be approximately 10 minutes of discussion afterwards.
This scenario focuses less on a clinical situation, and deals more with consideration of the moral, ethical, legal (etc.) issues which may arise in a situation.
The area of assessment here will be your suggested responses to the ethical scenario during discussion, as well as your knowledge of the different considerations required.
You will need to give a presentation on the following subject, for no more than 4 minutes:
'Why I am interested in a career in genitourinary medicine; and the evidence I have to support my suitability and commitment to the specialty.'
Specific guidance on preparing your presentation is given below:
'Unfortunately we cannot always offer a training post to all candidates and therefore, thinking about the length of your career to date, and the experience you have gained since qualification; please convince us in the four minutes allocated that the experience and skills you have gained in that time suggest you are worthy of a training post; your presentation will be timed.'
No aids/resources allowed – you are not allowed to use any visual representations, such as PowerPoint, when giving your presentation and you must not share your screen. You are welcome to use prompts on small cards, but these should be for your own use only.
When preparing your presentation, you should consider your career progression to date, achievements you have gained, examinations passed, competences, your portfolio, feedback received, etc.
Once your presentation is complete, your training, career to date and your suitability for the specialty will be discussed for approximately 6 minutes.
Scoring framework
The score of 1-5 an interviewer will award you for each assessment area is judged in relation to how well you perform against an expected level. Below is the framework used to award scores at interview, as well as interpretation of what these scores represent:
|
Mark
|
Rating
|
Assessment
|
|
1 |
poor |
not considered appointable |
|
2 |
area for concern |
performed below the level expected from a core level trainee applying to the specialty; |
|
3 |
satisfactory |
performed at the level expected of a core level trainee applying to the specialty; |
|
4 |
good |
above average ability; |
|
5 |
excellent |
highly performing trainee; |
As shown in the table, for each of the question areas at interview, 3/5 is considered a satisfactory score; and reflects the level of performance that would be expected of a trainee ready to progress to a specialty training programme.
Should your performance go above and beyond this expected level, interviewers can award marks of 4/5 or 5/5 as appropriate.
Conversely, should your interview performance not reach the expected level, then interviewers can award marks of 1/5 or 2/5, as reflects their level of concern over your performance.
Appointability
Raw interview score (RIS)
The RIS is the sum of all ten scores awarded to you during your interview, but before any weighting is applied.
As each individual score will be between 1 and 5, your RIS will be between 10 and 50.
Appointability requirements
To be classed as 'appointable', you must meet all three criteria below:
- none of your ten interview scores can be 1/5
- no more than two of your ten interview scores can be 2/5
- your RIS must be 30 or above.
If you meet all three requirements, your application will be assessed as appointable, and can progress to be considered for post offers.
However, if you fail to meet any of these requirements, your application must then be assessed as not appointable, and it will progress no further in that round.
Total score
After interview, a weighting is applied to the scores in each area, as well as your application score.
These scores are then combined to give your total score which determines your ranking, which will in turn be used to inform how offers are made. The weighting of different sections, as well as the method by which your total score is established, is detailed in the table accessible through the link below:
|
|
Interviewer 1
|
Interviewer 2
|
Weighting
|
Max score
|
|
Question 1 |
||||
|
Clinical scenario |
/ 5 |
/ 5 |
1.5 |
15 |
|
Communication |
/ 5 |
/ 5 |
2.0 |
20 |
|
Question 2 |
||||
|
Medical registrar suitability |
/ 5 | / 5 | 1.5 | 15 |
|
Question 3 |
||||
|
Ethical scenario |
/ 5 |
/ 5 |
1.0 |
10 |
|
Question 4 |
||||
|
Suitability & Commitment |
/ 5 |
/ 5 |
2.0 |
20 |
|
Raw interview score |
/ 50 |
|||
|
Interview score (w weighting) |
/ 80 |
|||
|
Application score |
/ 50 |
0.4 |
/ 20 |
|
|
Total score |
/ 100 |
|||